Introduction
Double-checking things is a common human behavior; we all do it. But what if you feel pressured to triple-check or even quadruple-check something? When these actions turn into an overwhelming need that disrupts daily life, it may be a sign of Obsessive-Compulsive Disorder (OCD). This mental health condition combines obsessive thoughts with compulsive behaviors, creating a cycle that significantly impacts one’s quality of life. People with OCD often recognize the irrationality of their behaviors but feel compelled to perform them, causing distress to themselves and those around them.
OCD is believed to affect about 2-3% of the population, which means millions of people worldwide struggle with this disorder every day. This article will explore OCD in depth, including its symptoms, potential causes, and the most effective treatments available. We aim to raise awareness and provide you with practical advice to help you or your loved ones manage this challenging condition.
What is OCD?
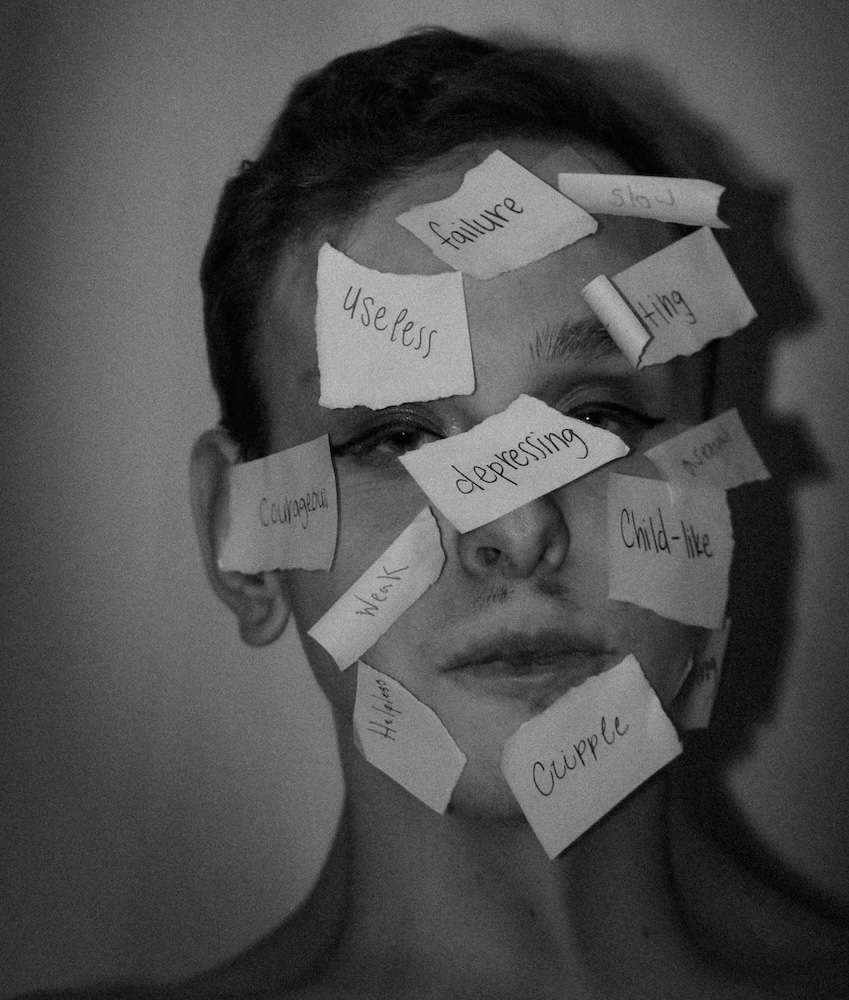
Obsessive-Compulsive Disorder (OCD) is a chronic mental health condition characterized by persistent, unwanted thoughts (obsessions) and repetitive behaviors (compulsions) performed to alleviate distress caused by these thoughts. These symptoms can interfere with daily life, social interactions, and overall well-being. People with OCD may find their days consumed by rituals and compulsions, leading to social isolation, anxiety, and even depression.
OCD and Its Impact on Daily Life
OCD can affect all aspects of an individual’s life. It often coexists with other disorders such as generalized anxiety disorder, depression, and even eating disorders. People with OCD are frequently misunderstood, leading to feelings of embarrassment and isolation. Unfortunately, stigma surrounding OCD can make it harder for individuals to seek help.
Symptoms of OCD
OCD is defined by two primary symptoms: obsessions and compulsions.
Obsessions
Obsessions are persistent, intrusive thoughts or fears that cause distress. Common types of obsessions include:
- Contamination Fears: An overwhelming fear of germs, viruses, bacteria, or environmental contaminants like chemicals and dirt.
- Doubts and Uncertainty: Constantly worrying about safety, such as whether doors are locked or appliances are turned off. Often accompanied by a need for perfectionism to avoid mistakes.
- Symmetry and Orderliness: An intense desire for objects to be aligned or arranged symmetrically, accompanied by discomfort when things are uneven or out of place.
- Unacceptable or Taboo Thoughts: Intrusive thoughts about harming oneself or others, inappropriate sexual thoughts, or extreme concerns about religious or moral correctness (scrupulosity).
Compulsions
Compulsions are repetitive behaviors or mental acts that individuals feel driven to perform to reduce the distress caused by obsessions:
- Cleaning and Washing: Excessive handwashing, cleaning objects or household items to the point of causing damage or distress.
- Checking Behaviors: Repeatedly checking locks, appliances, or safety devices, often seeking reassurance from others.
- Repeating and Counting: Performing actions a specific number of times or counting objects and steps to reduce anxiety.
- Arranging and Organizing: Constantly adjusting items until they feel “just right.”
- Mental Rituals: Silently repeating prayers or phrases, or replacing negative thoughts with neutralizing ones.
- Avoidance Behaviors: Avoiding people, places, or situations that might trigger obsessions, or hoarding to prevent imagined harm.
Transition: Now that we’ve discussed the primary symptoms of OCD, let’s dive into what might cause this condition to develop in the first place.
Causes of OCD
There is no single definitive cause of OCD; instead, it is believed to arise from a combination of genetic, biological, and environmental factors.
1. Genetic Factors
OCD often runs in families, suggesting a genetic predisposition. Research from the National Institute of Mental Health indicates that individuals with a first-degree relative (such as a parent or sibling) with OCD are twice as likely to develop the disorder themselves. Twin studies show that if one twin has OCD, the other twin is 45-65% more likely to develop it, especially in identical twins, confirming a strong genetic link.
2. Biological Factors
Neuroimaging studies have shown that people with OCD often have abnormalities in brain regions involved in regulating anxiety, such as the orbitofrontal cortex and basal ganglia. Additionally, serotonin, a neurotransmitter that helps regulate mood, anxiety, and repetitive behaviors, does not function properly in people with OCD. A disruption in serotonin levels can cause the brain to misfire, escalating the cycle of obsessions and compulsions.
According to a study published in the American Journal of Psychiatry, about 40-50% of people with OCD show improvements in symptoms when treated with selective serotonin reuptake inhibitors (SSRIs), confirming the role of neurotransmitter imbalances.
3. Environmental Factors
Environmental factors, such as trauma or stress, can trigger or worsen OCD symptoms. For example, individuals who have experienced severe accidents, illnesses, or abuse may develop OCD as a way to regain a sense of control. Research from the Journal of Anxiety Disorders suggests that early childhood trauma, such as emotional neglect or abuse, can increase the risk of developing OCD later in life by up to 30%.
Transition: Understanding the causes of OCD is crucial, but knowing how to manage and treat it is even more important. Let’s explore some of the most effective therapy methods currently available.
Therapy Methods for OCD
1. Cognitive Behavioral Therapy (CBT)
CBT is a highly effective and structured therapy that focuses on changing both cognitive (thought-related) and behavioral patterns. This therapy is particularly beneficial for those with OCD because it addresses the distorted thoughts that drive obsessions and compulsions.
- How CBT Works: Through CBT, patients learn to identify and challenge irrational or distorted thoughts and replace them with more realistic, balanced thinking. A typical course of CBT lasts 10 to 20 sessions, making it a cost-effective treatment option. This therapy has been shown to reduce OCD symptoms by up to 60% in many individuals.
2. Exposure and Response Prevention (ERP)
ERP is a specialized form of CBT specifically designed for OCD and is considered the most effective treatment for the disorder.
How ERP Works: ERP involves gradually exposing individuals to their obsessions (e.g., touching a doorknob perceived as contaminated) and preventing the subsequent compulsive behavior (e.g., not washing hands afterward). Over time, this exposure reduces the distress associated with the obsessive thought and breaks the cycle of compulsive behavior.
Effectiveness of ERP: Studies indicate that ERP can reduce symptoms by up to 70% in many patients and has long-lasting effects, even after the therapy has ended.
3. Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are a class of medications commonly prescribed to manage OCD symptoms. They help balance serotonin levels in the brain, making it easier for patients to benefit from therapies like CBT and ERP.
- Effectiveness of SSRIs: When combined with CBT or ERP, SSRIs can enhance treatment outcomes, leading to a reduction in OCD symptoms for up to 40-60% of patients.
4. Other Treatment Approaches
- Mindfulness-Based Cognitive Therapy (MBCT): Combines traditional cognitive therapy techniques with mindfulness strategies to help individuals focus on the present moment, reducing the power of obsessive thoughts.
- Deep Brain Stimulation (DBS): An option for severe, treatment-resistant cases of OCD, DBS involves surgically implanting electrodes to regulate brain activity. Though more invasive, it has shown positive results in some patients.
5. Best Treatment Combinations
Research suggests that a combination of ERP, CBT, and SSRIs is generally the most effective approach for treating OCD. However, the best method varies depending on the individual’s symptoms and response to therapy. A tailored approach is essential to meet the specific needs of each patient.
Transition: With several treatment options available, you might wonder how to choose the right approach for you or a loved one. Here are some frequently asked questions to help guide your decision.
FAQ: Living with OCD
Q1: Can OCD go away on its own?
A: While symptoms can fluctuate over time, OCD is generally a chronic condition that does not resolve without treatment. However, effective therapies like CBT and ERP can significantly reduce symptoms.
Q2: Is medication always necessary to treat OCD?
A: Not necessarily. While SSRIs can be helpful, especially for severe cases, many people benefit significantly from CBT and ERP alone. A mental health professional can help determine the best approach for each individual.
Q3: How long does it take to see improvement in OCD symptoms with therapy?
A: Many patients begin to see improvement within 10-20 sessions of CBT or ERP, though individual results may vary. Consistency and commitment to the therapy process are key factors in success.
Q4: Can OCD symptoms worsen over time?
A: Without treatment, OCD symptoms can become more severe. Stress, trauma, or other life changes may exacerbate symptoms. Seeking early treatment can help prevent worsening.
Q5: How can I support a loved one with OCD?
A: Be understanding and patient. Encourage them to seek professional help, and avoid enabling compulsions. Educate yourself about the disorder to better understand what they are going through.
Transition: Living with OCD can be incredibly challenging, but with the right support and treatment, individuals can manage their symptoms effectively and lead fulfilling lives.
Conclusion
Living with OCD can be difficult, but it’s important to remember that you are not alone. OCD is a common mental health disorder, and there are numerous effective treatments available. At Therapsy, we offer a range of evidence-based therapies, including CBT and ERP, tailored to meet your unique needs. Our experienced psychotherapists and psychiatrists are here to help you navigate your journey toward recovery.
If you or someone you love is struggling with OCD, don’t hesitate to reach out. Book a consultation with one of our mental health professionals today and take the first step towards regaining control of your life. Visit Therapsy.it to learn more about our services or schedule an appointment.
Remember, seeking help is a sign of strength, not weakness. There is hope, and with the right support, life can become manageable and enjoyable again.
If you’re ready to start your journey to wellness, reach out to us at Therapsy. Our team of dedicated psychotherapists and psychiatrists is here to provide the care and support you need. Contact us today at Therapsy.it to book your first session!
By understanding OCD and the available treatments, we can foster a more supportive environment for those affected and help them on their path to recovery.